Laser therapy for fungal nails? Does it really work?
I often encounter patients struggling with fungal nail infections (onychomycosis), a stubborn and frustrating condition. In recent years, laser therapy has gained attention as a potential treatment for fungal nails. It’s marketed as a quick, painless, and effective alternative to traditional treatments like oral antifungals or topical solutions.
But does the science back the claims? While laser therapy might seem like an appealing option, I remain sceptical about its efficacy as a stand-alone treatment for fungal nail infections. Here’s why.
Understanding Fungal Nail Infections
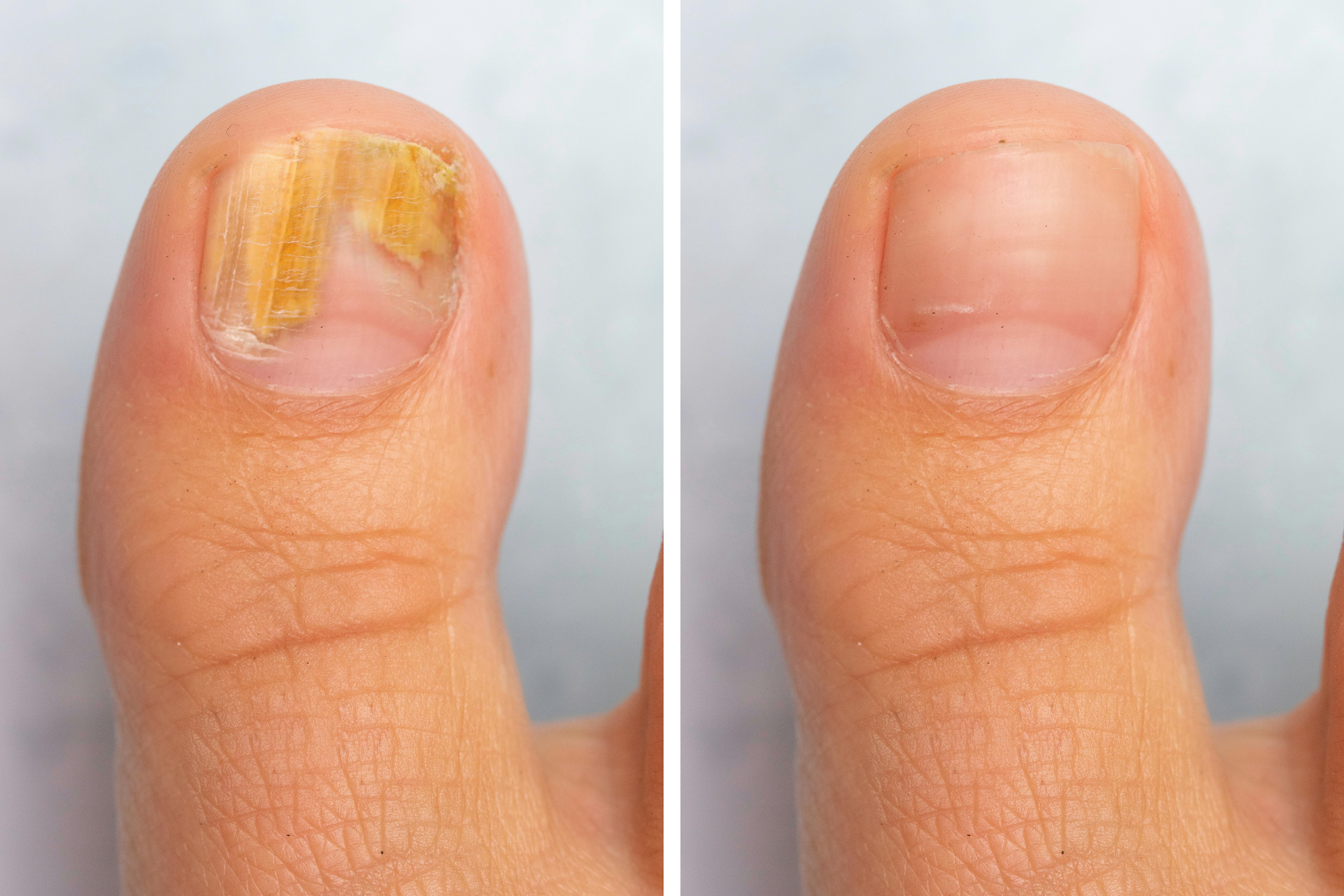
Fungal nail infections are caused by dermatophytes, yeast, or moulds that thrive in the warm, moist environment under the nail. These infections can lead to thickened, discoloured, and brittle nails, often causing embarrassment or discomfort for sufferers.
Treatment is often challenging because the infection lives beneath the nail, making it difficult for medications to penetrate. This is why traditional treatments, including oral antifungals, require a sustained and systematic approach.
How Laser Therapy Works
Laser therapy involves directing focused light energy at the affected nail. The theory is that the heat generated by the laser will kill the fungal pathogens without damaging the surrounding tissue. Practitioners who use laser for fungal nails will often claim benefits such as:
- Minimal discomfort during the procedure.
- No systemic side effects compared to oral antifungal medications.
- Shorter treatment durations compared to topical solutions.
The Reality: Where’s the Evidence?
While laser therapy sounds promising in theory, the clinical evidence supporting its efficacy is limited and often inconclusive. Here are some key issues:
- Inconsistent Results
Studies examining the effectiveness of laser therapy for fungal nails have produced mixed results. Some show modest improvements, while others report no significant difference compared to placebo treatments. - No Guarantee of Eradication
Even when laser therapy appears to clear the nail, there’s no guarantee that the fungal infection has been completely eradicated. Recurrence rates can be high, particularly if contributing factors like poor foot hygiene or untreated shoes aren’t addressed. - Lack of Standardisation
Different clinics use various types of lasers and treatment protocols, making it difficult to compare outcomes. There’s no universal guideline for the number of sessions required, the intensity of the laser, or how to combine it with other treatments. - Cost vs. Benefit
Laser therapy is expensive. When the results are uncertain, it raises questions about whether this investment is worthwhile compared to more established, evidence-based treatments.
Why I Prefer Evidence-Based Approaches
I believe in recommending treatments that have a strong foundation of clinical evidence. For fungal nail infections, this often includes:
- Oral Antifungal Medications
Medications like terbinafine (Lamisil) and itraconazole have a proven track record of success, particularly for severe infections. There are potential side effects, and not all will be able to take these drugs, but for many patients, the benefits outweigh the risks. - Topical Treatments
While less effective for severe infections, topical antifungal solutions can be a good option for mild cases or for patients who can’t take oral medications. - Combination Therapies
Combining oral and topical treatments can improve outcomes, especially when paired with regular podiatry care to debride (thin) the affected nails, improving medication penetration.
Laser Therapy as a Complementary Option
I’m not completely against laser therapy. It may have a role as a supplementary treatment for fungal nails, especially for patients who cannot tolerate oral antifungals. However, I view it as part of a broader treatment plan rather than a stand-alone solution.
For laser therapy to be effective, it must be combined with:
- Addressing Lifestyle Factors: Ensuring proper foot hygiene, regularly disinfecting footwear, and keeping nails trimmed.
- Regular Maintenance: Following up with debridement and potentially using topical treatments to prevent reinfection.
Final Thoughts
While laser therapy for fungal nail infections is an interesting development, it’s not the magic bullet it’s often made out to be. The evidence remains inconsistent, and it’s important to weigh the cost and benefits carefully.
If you’re considering laser therapy, I encourage you to discuss it with a qualified podiatrist who can help you understand the limitations and explore whether it’s the right option for you. In many cases, a combination of proven treatments, coupled with proper foot care, is still the best approach for tackling fungal nail infections.
If you’re struggling with fungal nails and want guidance on the most effective treatment for your situation, book an appointment. Let’s take a practical, evidence-based approach to restoring your nail health.